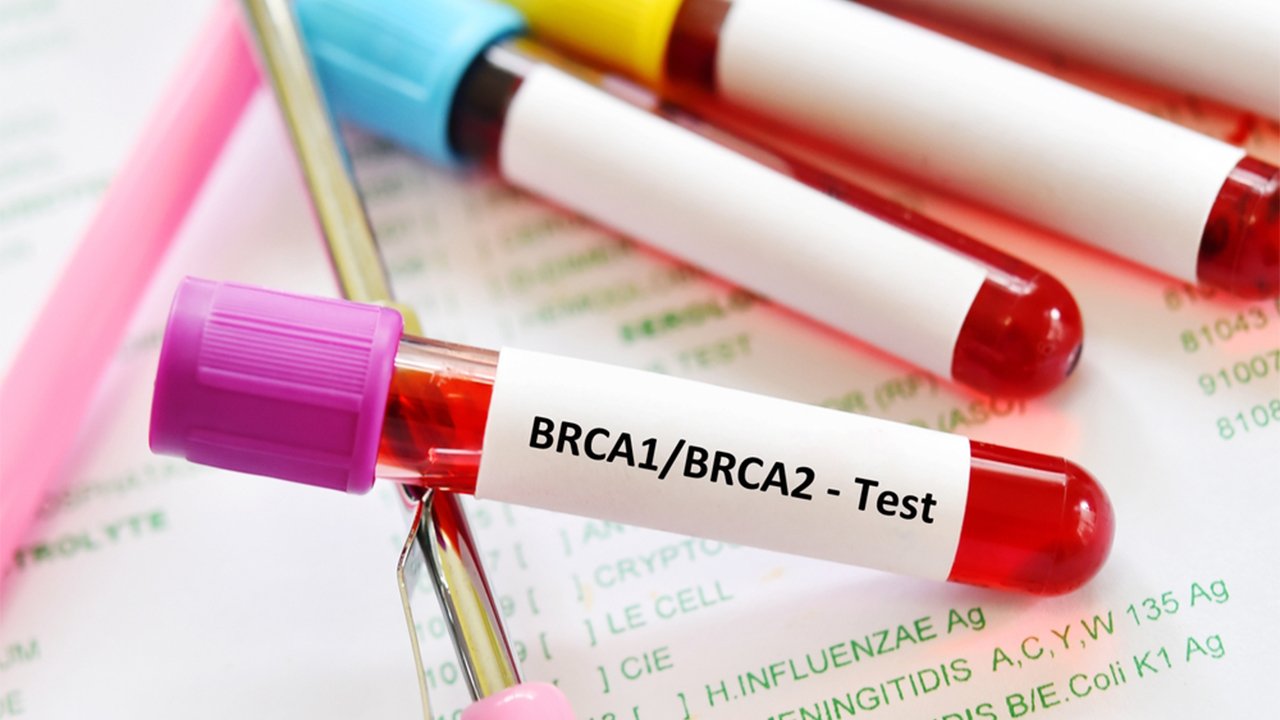
BRCA Gene Analysis in Breast Cancer
What is BRCA?
BRCA stands for “BReast CAncer Gene”. BRCA1 and BRCA2 are the two genes that are present in all human beings. These genes help in the repair of DNA breaks caused by different carcinogens, and thus, play a crucial role in the prevention of cancer. Any mutation or alteration in any one of these genes render them non-functional and may lead to the development of cancer, especially breast and ovarian cancer. An individual can pass-on the BRCA1/2 mutations to the next generation. The mutations in BRCA1/2 are the most common mutations responsible for familial breast cancer.
How is a mutation in the BRCA gene detected?
Several genetic tests are available for the detection of mutation in BRCA genes. These tests are generally known as DNA analysis. Some DNA analyses detect only a specific mutation (e.g. either BRCA1 or BRCA2) while some can detect multiple mutations (e.g. both BRCA1 and BRCA2) in one go. Next-generation sequencing can analyze all harmful mutations in the complete human genome, including BRCA1 and BRCA2. Thus, as per the patient’s requirements and discretion of the physician, an appropriate DNA analysis technique can be selected for the detection of mutation in the BRCA gene.
What is the significance of BRCA gene analysis?
BRCA gene analysis has substantial diagnostic and prognostic value. Inherited mutation in either BRCA1 or BRCA2 increase the chances of getting breast cancer. About 5% to 10% of all breast cancer patients and about 15% of all ovarian cancer patients have inherited BRCA gene mutations. According to another estimate, about 72% and 69% of women with BRCA1 and BRCA2 mutations, respectively, will develop breast cancer by the age of 80 compared to an estimated incidence rate of 12% in the normal population. Similar trends are anticipated for ovarian cancer with about 44% and 17% expected incidence rate in women with mutated BRCA1 and BRCA2 genes, respectively, compared to about 1.3% in the normal population. Mutation on BRCA gene has also been linked to an increased risk of some other cancers, for example, fallopian tube cancer, peritoneal cancer, pancreatic cancer, and prostate cancer.
A meeting with a genetic counselor is generally recommended before genetic testing. Such meetings help in resolving common concerns regarding the appropriateness of genetic testing, medical implications of a positive or a negative test results, and risks and benefits of genetic test results.
Who should consider BRCA gene analysis?
BRCA1 and BRCA2 gene mutation are rare in the general population. Thus, the analysis of BRCA1/2 gene mutation is not routinely performed and recommended for individuals who have one of the following attributes:
- Diagnosis of breast cancer at an early age (<50 years) in a woman or in a family member
- Diagnosis of cancer in both the breasts at the same time in a woman or in a family member
- Diagnosis of cancer in both the breasts and ovary in a woman or in a family member
- Multiple cases of breast cancer in the same family
- Breast cancer diagnosis in a closely related male (e.g. father or brother)
- Diagnosis of triple negative breast cancer at an age less than 60 years
- Diagnosis of ovarian cancer in a woman or in a family member
- Diagnosis of BRCA gene mutation in a family member
- Anyone of the following ethnicities: Ashkenazi Jewish, Norwegian, Dutch, and Icelandic peoples
In the case of breast cancer family history suggestive of BRCA gene mutation, it is generally recommended to test the first family member who had breast cancer. The test results will help in deciding whether other family members should be tested and what are the implications of genetic testing in other family members.
Genetic testing for BRCA gene mutation is not recommended for individuals below 18 years of age, because there are no established risk-reduction strategies for BRCA-associated cancers in this population.
What do BRCA gene analysis results mean?
BRCA gene analysis results are not always exclusive. The results obtained from BRCA genetic testing are divided into the following 3 categories:
1. Positive Results:A positive result confirms the presence of harmful mutations in the BRCA gene, which indicate an increased risk of developing breast and/or ovarian cancer. The positive results also have an implication on the next-generation who can inherit these mutations.
2. Negative Results: If an individual with a known family history of BRCA mutation associate breast/ovarian cancer has a negative test result, it is referred to as the true negative result. The true negative result indicates that the individual does not have any harmful mutation in the BRCA gene, and thus have the same risk of developing breast/ovarian cancer as that of the general population.
However, in the absence of a confirmed family history of BRCA mutation, negative results are difficult to interpret. Although rare, the genetic testing may have missed a known BRCA gene mutation or harmful mutations other than those recognized previously may be present, which could have been missed by the genetic test utilized.
3. Ambiguous Result: In about 10% of the cases, different mutations are detected in BRCA gene compared to those recognized previously as harmful mutations. Such results are known as ambiguous or of uncertain significance. Such mutations may prove to be harmful/harmless in near future.
What are the advantages of BRCA gene analysis?
BRCA gene analysis confers various advantages as described below:
The individuals with a positive result may discuss the results with a genetic counselor and/or an oncologist to make an informed decision about their prospective health-care, including steps to reduce the risk of cancer in future. Some individuals may choose to have a frequent screening starting from an early age compared to that suggested for the general population. Both American Cancer Society and the National Comprehensive Cancer Network, now recommend annual screening with mammography and MRI in women with increased risk of breast cancer. Some woman may choose to have a risk-reducing surgery (e.g. bilateral mastectomy–removal of both the breasts and/or bilateral salpingo-oophorectomy– removal of ovaries and fallopian tubes) to reduce the risk of cancer in future.
Researchers have demonstrated that bilateral salpingo-oophorectomy reduces the risk of dying from any cause by 77%. Also, some women may choose to use some drugs (e.g. tamoxifen, raloxifene, exemestane, anastrozole, and some oral contraceptives) for cancer risk reduction.
A person with BRCA gene mutation usually has an increased risk of developing cancer in both breasts, developing triple negative breast cancer, and developing second cancer. Also, the disease prognosis is poor in these patients compared to other patients.
Researchers have concluded that mutation in BRCA1/2 gene is usually associated with an increased risk of ovarian failure at an early age. Thus, individuals with BRCA1/2 gene mutation who wish to have children in the future should be given the option of embryo/oocyte cryopreservation.
Detection of BRCA gene mutation in a woman with breast cancer help in selecting an appropriate treatment strategy in these patients. Bilateral mastectomy should be employed in such patients even when they are candidates for breast-conservation surgery. PARP inhibitors, such as olaparib or rucaparib are approved for the treatment of patients with advanced ovarian cancer and BRCA1/2 mutations. Olaparib is also approved for the treatment of patients with HER2-negative, metastatic breast cancers, and BRCA1/2 mutation.
The individuals with a true negative result may have a sense of relief regarding the risk of developing cancer in the future.
You can also read: Symptoms and Signs of Brain Cancer
What are the limitations of BRCA gene analysis?
The BRCA gene analysis may have harmful effects on the person’s emotions, finances, social relations, medical choices, and life choices (e.g. decisions about career, marriage, and childbearing). People may develop intense anger, depression, or anxiety, especially after the genetic analysis test results are out and are positive. People may find it difficult to choose a cancer risk reduction approach that suits them the most.
Although very small, there are chances of false-positive or false-negative results, which can have various adverse consequences on a person’s life.
BRCA is not the only gene that predisposes an increased risk of developing breast cancer. There are several other genes that can increase the risk of developing breast cancer, for example, PALB2, TP53, CDH1, and CHEK2. Testing for a mutation in these genes requires additional genetic testing or initial testing required to be performed by multiple panel testing/ next-generation sequencing.